Sciatica is a condition which results in pain radiating through the lower back, the back of the thigh and down to the foot. Though we do assist patients with this condition, there are also quite a few patients who come to the clinic thinking that sciatica is what’s causing their pain, only to find out that their pain is a result of something entirely different. In today’s article osteopath Chloé Sardin will explain what causes sciatica and explore other conditions and imbalances that can cause pain in the lower back.
 During the cold winter months, we often see more patients being affected by neuralgia (nerve pain) of the lower back, and legs, which might have to do with the cold contributing to more muscle tension and accidents both by car and on foot.
During the cold winter months, we often see more patients being affected by neuralgia (nerve pain) of the lower back, and legs, which might have to do with the cold contributing to more muscle tension and accidents both by car and on foot.
Here are 6 common myths about sciatica and your lower back’s health:
1. The acute pain in my leg feels like a nerve, so it must be sciatica.
The lower back has many nerves exiting the spinal cord and going towards the legs. They are each responsible for the mobility of certain muscles and the sensitivity of a skin area of the leg. When a patient talks to us about a pain we use our knowledge to figure out which “root” of nerves is affected, and which branch of it could be related to the symptoms. Maybe it is because sciatica is known to be one of the most excruciating pains a human can have, we often have patients coming for sciatica pain that isn’t sciatica.
 Here are the more common nerve pains in the pelvis/leg area:
Here are the more common nerve pains in the pelvis/leg area:
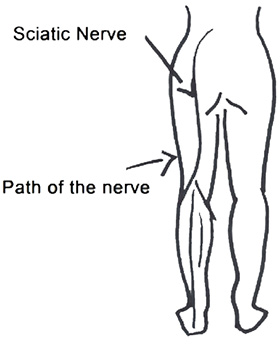
- Sciatic nerve: Irradiating pain from the lower back to the back of the thigh all the way to the foot.
- Lateral Cutaneous nerve of the thigh: Like its name indicates it affects the front and lateral part of the thigh.
- Inguinal nerve: Bothers the inner thigh.
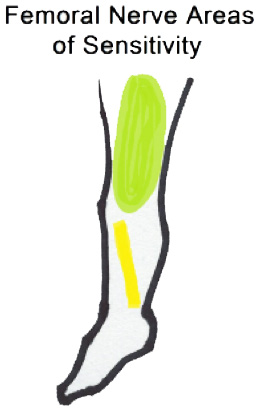
- Femoral nerve: Ache on the upper thigh on the front, and inner part of your leg.
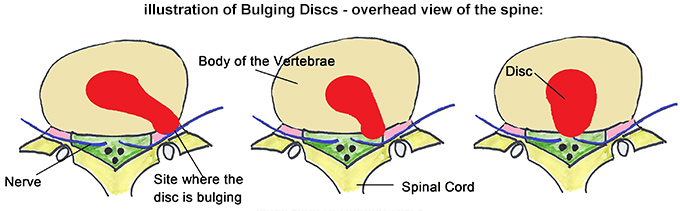
2. Sciatica only has one cause: bulging discs.
As manual practitioners, we actually distinguish 2 types of sciatica:
- The True Sciatica: caused by a bulging disc, arthritic changes in the lumbar spine, or more rarely by other causes like infections or tumors. Patients will describe a sudden agonizing pain on one side behind their leg which prevents them from sleeping, causes tingling, shooting pain, or numbness in the back of their thigh. The pain gets worse when they stand or do anything physical, especially coughing or sneezing (causes an increase of pressure on the nerve).
- The Pyramidal Syndrome: caused by the sciatic nerve compression or irritation by the pyramidal muscles (part of the gluteal muscles). Because of its location, the sciatic nerve is either in front of this muscle in the pelvis or in 15% of patients, it goes through the muscle and when the muscle spasms or gets thick it will bother the nerve. The pain will be similar to true sciatica but starts more gradually, often occurring after overuse of the glute muscles or after long periods of sitting such as driving, travelling, working long hours (the muscles naturally get tight in this position, and the body weight is sitting on the nerve), any external rotation of the hip (which is its job), palpation of the muscle, or turning in bed will worsen the pain. It is very important for health practitioners to have the right diagnosis in order to treat the cause of the problem.
3. Medical Imagery (x-rays, MRI, CT scans) results are proportional to my level of pain.
In order to compress a nerve exiting the spinal canal, a hernia must be a significant size to compress it. Moreover, different studies show that the majority of the “symptom free” population is actually affected by disc protrusion (sticking out) and arthritic/degenerative changes.
There are suggestions that those changes are a normal part of getting older, and not related to the pain patients are experiencing. Your last “bad x-ray” doesn’t mean you should be in pain, and reciprocally if no medical exams have found anything, it does not mean the issue is psychosomatic (in your head).
Pain levels are related to the context (where did the accident happen), what mindset we were in at that time (tired, stressed), past experiences, and degree of nerve irritation (pain levels fluctuate greatly from person to person). But let’s say you are a professional musician–hurting your hand will be a big deal for your career and the pain level will be influenced by it. And say if an entrepreneur is bedridden because of back pain–this just isn’t an option sometimes.
 4. Manipulation of the vertebrae will decompress the nerve and make the pain go away.
4. Manipulation of the vertebrae will decompress the nerve and make the pain go away.
As discussed previously, sometimes muscles can cause nerve entrapment (strangling). Now, as osteopaths believe that the body works as a whole, an adaptation will likely occur elsewhere in the body to try to help you. During an osteopathic treatment for sciatica, for example, we will check your legs, pelvis, and spine, but also make sure muscle asymmetries are not getting in the way or pulling your back (like the diaphragm or the psoas, which is a powerful hip flexor). Furthermore, we will check that your guts aren’t dragging your lower back forward through their attachment in front of the body of the vertebrae.
Finally, the lower back works in team with the cervical spine (neck) as they share the same shape (C-shape called lordosis), and the base of the skull mimics the shape of the pelvis, therefore we will check any compensation higher up in your body.
5. It must be the mattress, or it happened out of nowhere.
Things don’t happen without a reason and nerve pain is no exception. There are cumulative processes leading to our pain/disease and symptoms, there is never a one and only cause. Therefore, being tired, stressed, over exercising, being overweight, pregnancies, a weak core, can all contribute to your question: why now?
6. I am in so much pain… the more treatment and therapies, the better.
Actually, more is not always the better. Each treatment and each practitioner works (maybe differently) on your body–the same body. This requires that your body responds/adjusts to it locally, but also generally, and your nervous system interprets those changes (which takes at least a couple of days). The accumulation of new information and changes can become overwhelming and cause an “overtreatment” where the body stops responding to treatment or can actually increase the symptoms momentarily. This is one of the reasons why we ask patients to space out their treatments to give the body a chance to respond appropriately.

What can you do to get better faster, then? Some strengthening of the core muscles (not the hip flexor, as it can cheat by helping out a bit too much!), and stretching or strengthening of the glutes. Make sure food isn’t causing more inflammation, work on your breathing in order to stretch the lumbar attachments of the diaphragm, and ask your Osteopath for advice that’s tailored to you, specifically.
If this interests you, you might consider booking an appointment with me here.
